Understanding Managed Care
Managed care involves managing healthcare services to improve quality and control costs.
This approach includes diverse plans like HMOs, PPOs, and EPOs, each with unique features and benefits.
History and Evolution
Managed care began to gain traction in the 20th century.
One key moment was the development of Health Maintenance Organizations (HMOs).
President Nixon signed the Health Maintenance Organization Act in 1973, which promoted the growth of these plans.
Over the years, managed care expanded to include other plans like Exclusive Provider Organizations (EPOs) and Preferred Provider Organizations (PPOs).
Changes in law and policy also influenced managed care, making it a significant part of modern healthcare.
Types of Managed Care Plans
There are several types of managed care plans, each with unique features. Health Maintenance Organizations (HMOs) require members to choose a primary care physician and get referrals for specialists. Preferred Provider Organizations (PPOs) offer more flexibility, allowing members to see any doctor within the network without referrals.
Exclusive Provider Organizations (EPOs) are similar to PPOs but typically do not cover out-of-network care except in emergencies. Point of Service (POS) plans combine aspects of HMOs and PPOs, offering some out-of-network coverage with higher costs.
Managed Care vs. Fee-For-Service
Managed care and fee-for-service are different approaches to healthcare.
Managed care focuses on controlling costs and optimizing care.
Plans often have networks of providers and emphasize preventive care.
Financial incentives are used to keep costs down and improve quality.
Fee-for-service, on the other hand, pays providers for each service they perform.
This can lead to more tests and procedures, driving up costs.
Managed care systems aim to reduce unnecessary services and encourage efficient care delivery through coordinated efforts.
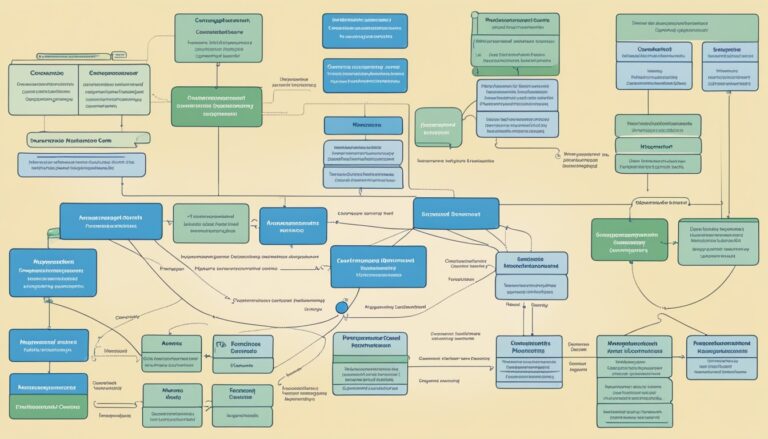
Managed Care Operational Framework

Managed care is designed to provide efficient and cost-effective healthcare through provider networks, specific payment models, and rigorous quality and utilization reviews.
This framework ensures patients receive necessary care while managing healthcare expenditures.
Provider Networks and Payment Models
In managed care, provider networks are groups of doctors, hospitals, and other healthcare providers who have agreed to offer services at reduced rates.
As a member, you must typically see an in-network provider to benefit from lower costs. Payment models in managed care include:
- Capitation: Providers are paid a set amount per patient regardless of the services provided.
- Fee-for-service: Payments are made for each service rendered.
- Cost-sharing: Patients pay a portion of costs through methods like co-pays and deductibles.
These models create economic incentives to control costs while ensuring medical necessity.
Cost Management Strategies
Managed care plans use various cost management strategies to maintain affordable healthcare. Utilization management ensures that services are medically necessary. Case management helps coordinate care, especially for those with complex health needs.
Other strategies include:
- Gatekeeper: Often a Primary Care Provider (PCP) who controls patient access to specialists and additional services.
- In-network vs. Out-of-network: Patients pay more for out-of-network services to encourage the use of in-network providers.
- Co-pays: Fixed amounts patients pay for certain services, which differ from deductibles (learn more about co-pays).
These strategies prevent unnecessary expenditures and keep healthcare costs down.
Quality and Utilization Review
Ensuring quality care is central to managed care. Utilization review involves evaluating the necessity, efficiency, and appropriateness of healthcare services provided.
This review process includes:
- Pre-certification: Approving services before they are provided.
- Concurrent review: Ongoing assessment during treatment.
- Retrospective review: Evaluating care after treatment has been given.
These reviews help maintain high standards of care while keeping costs in check.
They also guide decisions on medical necessity and help to avoid unnecessary treatments.
Additionally, quality of care is continuously monitored to ensure patients receive effective and safe treatments.
Challenges and Innovations in Managed Care

Managed care faces numerous challenges that impact its effectiveness and growth.
Key issues include navigating regulatory compliance, integrating technological advancements, and addressing future trends in healthcare.
Regulatory Challenges and Compliance
Managed care organizations must comply with a myriad of regulations to maintain their operations.
Changes in healthcare laws, such as the Affordable Care Act, require ongoing adjustments to policies and services.
Health insurance companies need to ensure that their health plans meet the standards set by accreditation bodies like NCQA, which helps in maintaining the quality of care.
Compliance with regulations often involves meticulous documentation and evidence to demonstrate adherence to standards and improve patient trust.
Selective contracting with healthcare providers is another challenge.
Organizations must balance cost and quality, often involving negotiations that ensure coverage meets regulatory requirements without compromising care.
Technological Advancements
Technology is revolutionizing managed care.
Health insurance companies are adopting advanced data analytics to improve outcomes and reduce healthcare costs.
The use of electronic health records (EHR) enhances coordination between providers and patients, fostering better patient care services.
Telehealth has emerged as a crucial innovation, especially for special needs plans and long-term care services.
It provides quicker access to primary care physicians, improving the quality of care and preventive care options.
Innovations like artificial intelligence (AI) are also being used to streamline prior authorization processes, reducing delays in patient care.
Value-based care models benefit significantly from technology, enabling better tracking of healthcare quality and ensuring that the right care is delivered at the right time.
Future of Managed Care
The future of managed care is set to evolve with the growing emphasis on patient-centered models and public health initiatives.
Managed care organizations are likely to focus more on social determinants of health, addressing factors like housing, education, and food security, which impact healthcare outcomes.
Competition among health plans is expected to increase, driving improvements in health care benefits and choices available to patients.
Medicaid programs are also likely to expand their coverage, integrating more value-based care approaches to enhance patient outcomes.
Technological advancements will continue to shape the future, with innovations aimed at reducing healthcare costs and improving overall population health.
This forward-thinking approach ensures that managed care adapts to emerging healthcare needs and challenges.